Ending HIV Transmission in Scotland by 2030: HIV Transmission Elimination Delivery Plan 2023-26
A detailed delivery plan outlining prioritised actions for the elimination of HIV Transmission in Scotland by 2030.
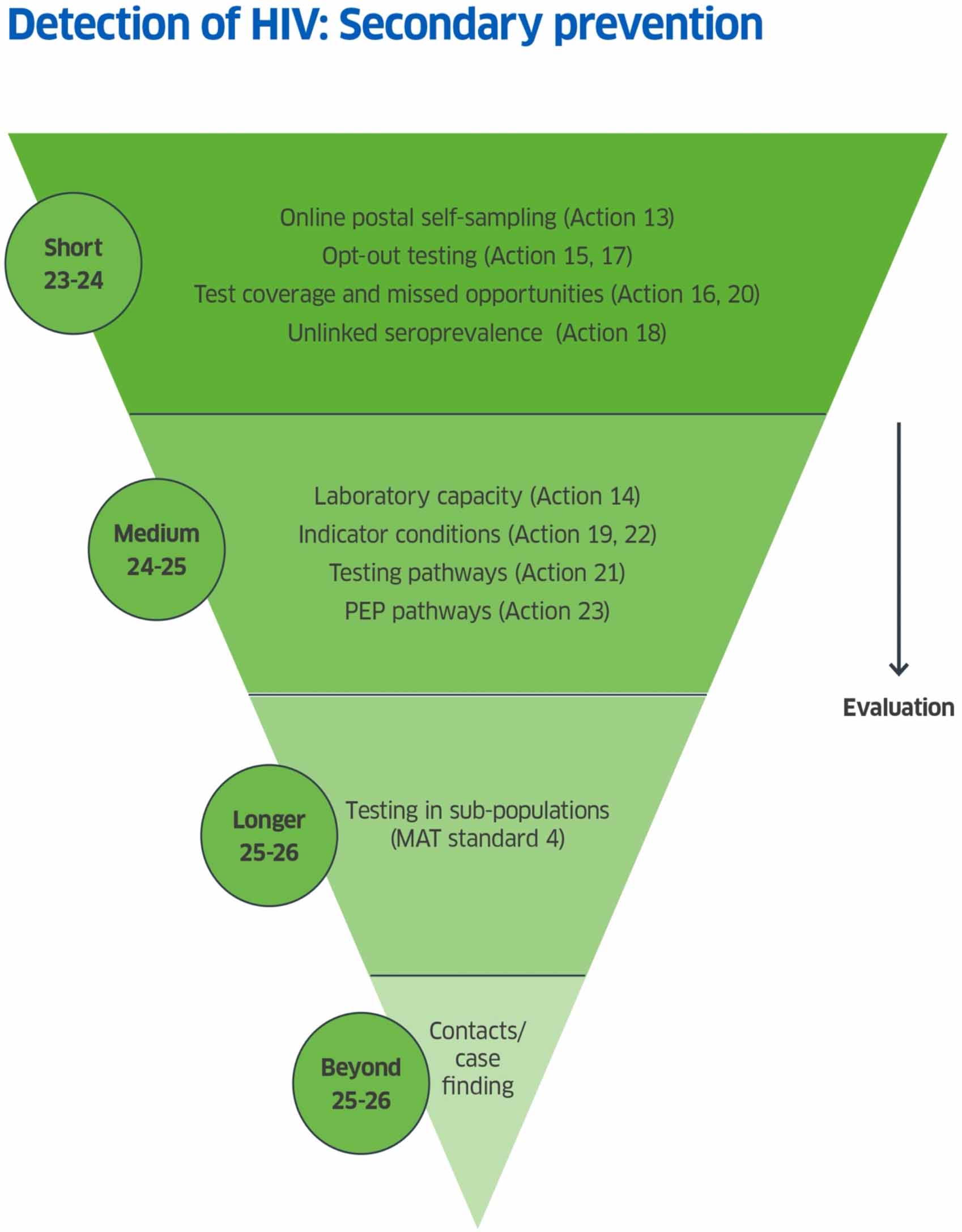
Secondary Prevention - Detection of HIV
Secondary prevention is the detection of HIV by the offer and acceptance of an HIV test. It incorporates actions to maximise the accessibility of testing, to make testing acceptable and equitable, and to ensure that when someone is diagnosed with HIV, their sexual partners and other contacts at risk are reliably and consistently identified and offered testing.
Secondary Prevention Actions
HiTEOG 1.1: To increase HIV testing coverage in specialist sexual health services in Scotland from 2023 onwards.
Action 13: A national Online Postal Self-Sampling service involving central procurement of test kits and national coordination of test order and delivery with some centralised results management will be developed.
Delivery by: PHS
Timeline: Short term Commence: October 2023 Complete by: March 2025
Detail: Several NHS Boards offer limited postal HIV testing locally. It is recognised that a centralised national Online Postal Self-Sampling (OPSS) service will provide a more cost-effective, consistent approach across Scotland.
As outlined in the SHBBV Action Plan, a centrally coordinated OPSS service for sexually transmitted infections including HIV is being taken forward by PHS in conjunction with the Diagnostics Strategic Network. This will provide a national service involving central procurement of test kits and national coordination of test order and delivery, with some centralised results management supporting delivery by local sexual health services and labs within existing local resources. Some gains in testing capacity will be made through the resourcing and implementation of a national system and the possibilities for further capacity increases at a national level will be explored over 2024/25. Additionally, a national HIV self-testing service has been funded by Scottish Government since 2020 providing self-testing kits via an online ordering system now hosted by THT[xvi]. This provision should continue to be offered in order to widen access to HIV testing.
HiTEOG 1.2: To provide sufficient laboratory capacity to support expanded BBV testing and confirmation activity from all providers in Scotland.
Action 14: Establish the capacity for and costs of BBV testing in Scottish laboratories.
Delivery by: Diagnostics Strategic Network and Scottish Microbiology and Virology Network with support from PHS
Timeline: Medium term Commence: April 2024 Complete by: 2025/26
Detail: Current total HIV/BBV testing capacity and requirements across lab services in Scotland is unknown. In conjunction with work to establish a national OPSS, discussions with the newly formed Diagnostics Strategic Network (DSN) and Scottish Microbiology and Virology Network (SMVN) will establish the current and potential laboratory capacity for HIV testing and models for delivery. This will establish what the required laboratory capacity for HIV (and other BBVs) currently is across Scotland, what we might expect demand to be if we reach the levels of testing required, how it is best delivered and at what cost.
HiTEOG 1.3: To increase BBV testing coverage to people in custody including those already in Scottish prisons reaching 90% uptake within the previous 12 months by December 2024.
Action 15: Support the delivery of a Target Operating Model (TOM) to include opt-out BBV testing for Scottish Prisons.
Delivery by: National Prison Health Network Programme Team.
Timeline: Short term Commence: 2023/24 Complete by: December 2025
Detail: National Prison Health Network Programme Team have finalised a TOM for prison healthcare and are currently convening a Sexual Health in Prisons forum to support delivery.
Guidance to support opt-out BBV testing in prisons was issued by PHS in July 2019[xvii]. HIV tests should be recommended to everyone in custody unless they are already known to be HIV positive or have been tested within the previous year and have not been at risk of transmission. A key foundation is to establish a national indicator of testing rates in prison along with linked and reported data for monitoring progress. It is recognised that the target of 90% uptake in the 12 months to December 2024 set in the original HiTEOG report is unlikely to be achieved and therefore a revised target has been set for completion.
HiTEOG 1.4: To offer universal opt-out BBV testing in Scottish drugs services by December 2024.
Action 16: Monitor BBV test coverage among people who inject drugs in Scotland through an automated approach that can be applied nationally in the future.
Delivery by: Glasgow Caledonian University and PHS
Timeline: Short term Commence: December 2023 Complete by: March 2025
Detail: Despite the wide provision of harm reduction interventions following the HIV outbreak in people who inject drugs in Glasgow in 2015, routine opt-out testing in drugs and alcohol services varies across the country. In some NHS Boards, opt-out testing has been adopted and services (including prisons) are expected to implement the Medication Assisted Treatment (MAT) standards for Scotland[xviii]
MAT standard 4 states that all people are offered evidence-based harm reduction at the point of MAT delivery; 4.2 states services should have a procedure in place to offer hepatitis and HIV testing and hepatitis B and tetanus, flu and COVID-19 vaccination, using an opt-out approach with regular follow-up as per local protocols.
Despite opt-out testing models and work around MAT standards, suboptimal proportions of those in receipt of OAT have evidence of recent BBV testing. Current MAT 4 data collection and clinical systems within addiction services do not include BBV testing as a reportable activity, so a key first foundation is to establish a national indicator of testing rates. Currently, comprehensive HIV laboratory test data is only available for NHS Greater Glasgow and Clyde. GCU have been funded in collaboration with PHS to monitor test coverage. The monitoring data will form the foundation for increasing testing in drugs services, work which will be delivered by NHS Boards and overseen by HIV-TEDI. The sharing of best practice will be key towards a nationally consistent approach. It is also important to ensure that this workforce is trained in HIV to ensure accurate and non-stigmatising support from staff in drugs services.
HiTEOG 1.5: To pilot HIV opt-out testing programmes in urban emergency departments where the diagnosed population HIV prevalence exceeds 1 in 500 people.
Action 17: Scottish Government to provide funding for small pilots of opt-out testing in Emergency Departments.
Delivery by: NHS Boards with Scottish Government funding
Timeline: Short term Commence: December 2023 Complete: June 2024
Detail: Opt-out emergency department (ED) testing for BBVs in five cities in England illustrates the effectiveness of the intervention, both in identifying new infections and re-engaging individuals in care, in very high prevalence areas[xix]. It also underlines the necessity of including tests for hepatitis B and C as well as HIV and the volume of testing required to identify significant numbers of undiagnosed individuals. Short pilots will be carried out within Scotland in late 2023 and early 2024 with reporting and evaluation into mid-2024. The evaluation data, combined with the findings from England and from the unlinked seroprevalence testing outlined below, will help determine whether opt-out ED testing is acceptable, deliverable and cost-effective in Scotland.
Action 18: PHS to scope and cost an Unlinked Anonymous Seroprevalence Testing programme for BBVs including HIV.
Delivery by: PHS
Timeline: Short term Commence: December 2023 Complete: March 2025
Detail: In order to establish extent of undiagnosed HIV infection in Scotland, and determine which areas in Scotland, if any, reach the cost-effectiveness prevalence threshold for HIV opt-out testing in EDs, an unlinked seroprevalence study should be carried out. PHS will scope and cost this work and HIV-TEDI will provide recommendations on next steps on taking this forward during 2024/25.
HiTEOG 1.6: To support health care workers to test people for HIV in the presence of an HIV indicator condition.
Action 19: A project to highlight indicator conditions to healthcare workers to be developed. This may be incorporated in other work on HIV education.
Delivery by: HIV-TEDI, Scottish Government, PHS and NES.
Timeline: Medium term Commence: April 2024 Complete: 2025/26
Details: Testing for HIV in people who present with a medical condition known or suspected to be associated with an underlying HIV prevalence of 1/1000[1] offers the possibility of improving rates of diagnosis particularly in low prevalence geographical areas where universal testing approaches are not cost-effective. Achieving a consistent and effective approach across health systems has proved particularly challenging despite a plethora of initiatives across the UK and internationally over three decades.
UK-wide implementation guidance to support the existing HIV/British Infection Association Adult HIV Testing Guidelines[xx] is in development. NHS Education Scotland (NES) is working to update materials and training targeted at healthcare practitioners in non-HIV specialist roles and a specialist educator post has been funded by Scottish Government to support the provision of training across Scotland. This project includes raising awareness of the need for HIV testing in those with indicator conditions.
Scotland’s size, integrated NHS system, independent clinical educational establishments and professional Royal Colleges offer an opportunity for a whole system improvement-by-design approach to Indicator Condition testing. A model including consistent messaging, patient and public facing information, linkages to professional bodies and guidelines, a portfolio of healthcare worker educational materials, prompts on laboratory and clinical systems and mechanisms to feedback and review testing rates will be delivered through professional training, workforce continuous professional development (CPD) and directly on the ground in Medical Assessment Units, Emergency Departments and in General Practice.
HIV-TEDI will lead expert discussion to advise Scottish Government on developing this coordinated approach to Indicator Condition testing. An important priority for Indicator Condition testing will be the inclusion of General Practitioners (GP), other primary care teams including Advanced Nurse Practitioners, other nursing and dental professionals and pharmacists in education and awareness raising activities.
Action 20: Investigate missed opportunities for testing in people diagnosed in Scotland and inform the future testing strategy.
Delivery by: Glasgow Caledonian University (funded by Scottish Government)
Timeline: Short term Commence: October 2023 Complete: March 2025
Details: An academic research study is underway to analyse routine test and diagnosis data and healthcare delivery data for people who have either had a late BBV diagnosis, or no evidence of a BBV test in the 24 months prior to diagnosis (including those who have never been tested). This work will inform evidence-based interventions for BBV testing.
HiTEOG 1.7: To evaluate HIV testing capacity and modalities by all providers in Scotland[2].
Action 21: Review modalities and pathways to HIV testing by all providers.
Delivery by: HIV National Coordinator (see action 24) supported by HIV-TEDI and HIV Clinical Leads.
Timeline: Medium term Commence: 2024/25 Complete: March 2025
Detail: In addition to HIV testing on blood samples taken in healthcare settings and Online Postal Self Sampling, the Scottish Government funds Terrence Higgins Trust Scotland to provide a national HIV self-testing service free to all Scottish residents. The service delivers blood-based or oral fluid-based home testing kits via an online ordering portal.
Third sector partners and NHS services also offer a range of outreach testing for groups and individuals who experience barriers to accessing mainstream services using supervised near-patient testing for HIV. Dried Blood-Spot testing is widely used in Drugs & Alcohol services and in some other settings. In parallel with establishing the laboratory capacity for HIV testing in Scotland, there is a need for a comprehensive overview of testing modalities and pathways in Scotland, to ensure professionals and the public have the knowledge and awareness of testing options available and in order to facilitate a more strategic approach to optimising capacity to meet demand.
HiTEOG 2.1: To routinely prompt consideration of HIV on laboratory result reports where the condition is a possible differential diagnosis of HIV.
Action 22: Develop a system of standardised laboratory prompts through the national laboratory informatics system.
Delivery by: NHS Boards and NHS NSS Laboratory Informatics System team with HIV Clinical Leads and HIV-TEDI.
Timeline: Medium term Commence: April 2024 Complete: March 2025
Details: The introduction of a National Laboratory Informatics System (LIMS) to the majority of NHS Boards in Scotland offers the opportunity to introduce a comprehensive and standardised set of prompts to HIV testing, triggered by both test requests (i.e. clinical conditions) and abnormal test results. The national LIMS implementation team have initiated discussions on the possibilities for delivering such a system, which would be supported by appropriate educational materials and pathways through actions 1 and 19.
HiTEOG 3.5: To update local HIV post-exposure prophylaxis (PEP) care pathways to be consistent with current guidance.
Action 23: Review and collate local HIV PEP care pathways to confirm that these are consistent with current BASHH-BHIVA guidelines in all NHS Boards.
Delivery by: SHPN Sexual and Reproductive Health (SRH) Clinical Leads & HIV Clinical Leads.
Timeline: Medium term Commence: April 2024 Complete: October 2024
Detail: The current BASHH-BHIVA UK guideline for the use of HIV post-exposure prophylaxis (PEP) was published in 2021[xxi]. PEP provision is a routine element of care across specialist sexual health services and Emergency Departments across Scotland. Local guidance should be in line with these national guidelines.
Contact
Email: SHBBV@gov.scot
There is a problem
Thanks for your feedback