Ending HIV Transmission in Scotland by 2030: HIV Transmission Elimination Delivery Plan 2023-26
A detailed delivery plan outlining prioritised actions for the elimination of HIV Transmission in Scotland by 2030.
Primary Prevention
Primary prevention includes awareness raising, information and education for the wider population, plus access to pre-exposure prophylaxis for HIV (PrEP), post-exposure prophylaxis (PEP), condoms, clean injecting equipment provision (IEP) and other interventions to support people who inject drugs such as Medication Assisted Treatment (MAT) including Opiate Agonist Therapy (OAT). These support associated behaviour change interventions for those at higher risk of acquiring HIV. Particular attention is required to groups and sub-populations with a higher prevalence of HIV and other risk factors, who may encounter barriers to uptake of prevention interventions. If the declining trajectory of HIV incidence continues, future efforts should be aimed at providing interventions in a more intensive and focused way to communities in which new HIV transmissions have occurred.
It continues to be vital that we address HIV stigma both for the benefit of people living with HIV in Scotland, as well as to underpin testing and prevention interventions. Education and information actions for the wider population, and for the Health and Social Care workforce, will therefore remain a priority.
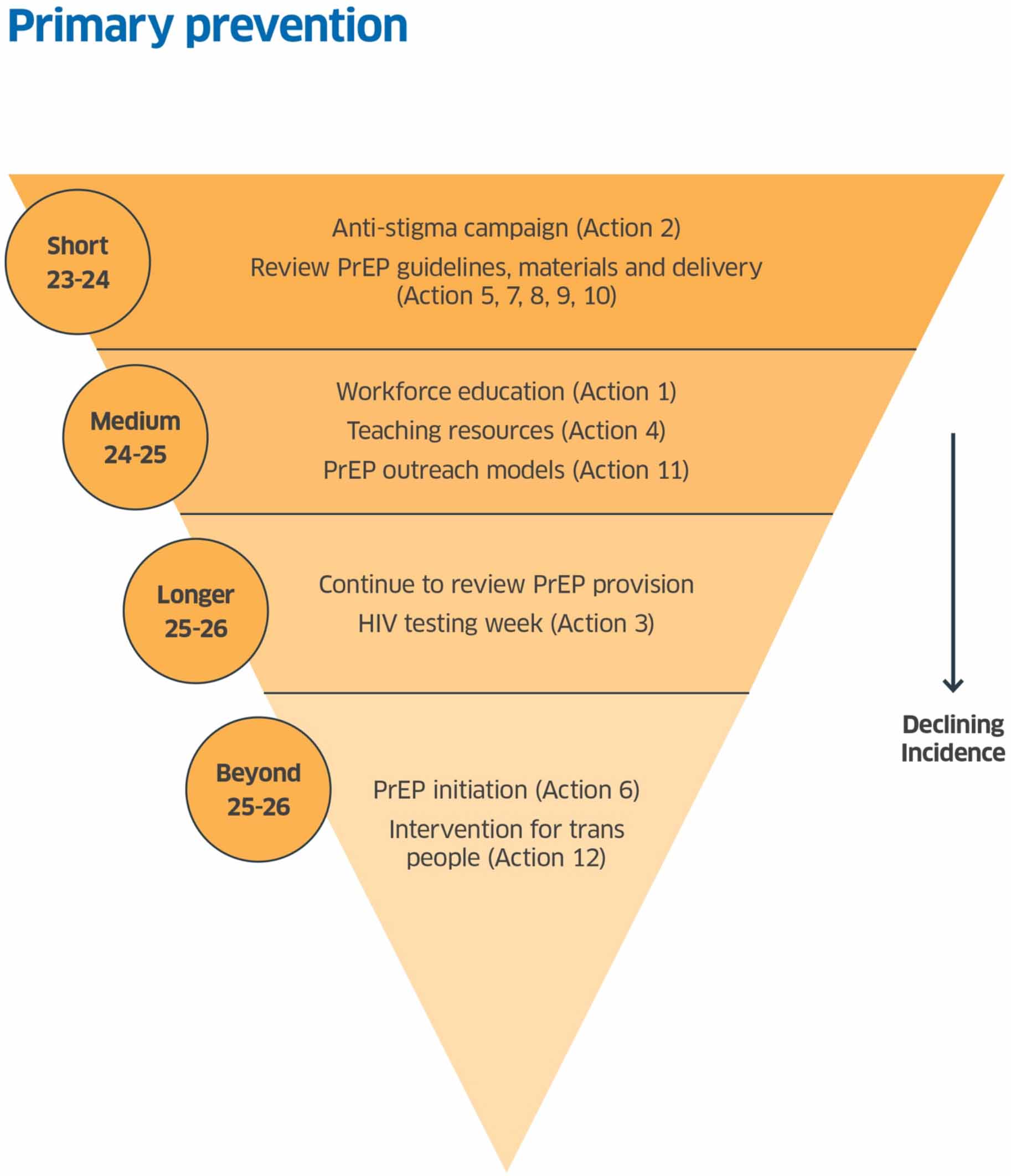
Primary Prevention Actions
HiTEOG 2.2 Provision of training (with support from HIV third sector organisations) to highlight HIV risk reduction for primary and secondary care clinicians.
HiTEOG 2.3: To support health and social care worker knowledge about the realities of HIV in the era of effective therapy and prevention.
Action 1: A proposal will be developed to address educational needs across the Health and Social Care sector, to be delivered in conjunction with other key actions.
Delivery by: Scottish Government, NHS Education for Scotland (NES) and others.
Timeline: Medium term Commence: April 2024 Complete: March 2025
Details: HiTEOG recognised that some non-specialist health and social care professionals have gaps in knowledge despite the large amount of progress made in treating and preventing HIV since the 1980s. Lack of up-to-date knowledge may exacerbate stigma and lead to inappropriate behaviour in relation to concerns about infection control. The engagement of people living with HIV in the anti-stigma campaign already underway, along with the lived experience panels associated with the Fast Track Cities consortium[vi], has continued to flag that some targeted work on stigmatising behaviours is required in the Scottish health and social care system.
This action will address recommendations 2.2 and 2.3 and will also encompass elements of other key recommendations: Indicator Condition testing (particularly relating to general practice) (1.6), PrEP prescribing guidance (3.1), and prevention after a negative test (4.2). The objective of this action is to support multidisciplinary teams outside specialist settings with knowledge, skills and attitudes to assess and discuss individual HIV risk and to facilitate appropriate testing and interventions to reduce future risk.
The public anti-stigma campaign (2.4) provides a foundation for more targeted information provision. A tiered approach will equip the Health and Social Care workforce and others, including those working in education and elsewhere, with the knowledge and skills to support a more localised approach to primary prevention, testing, treatment and care and will be fundamental to success. Addressing stigma within the Health and Social Care workforce is also critical to ensure that the care needs of people living with HIV in Scotland are properly addressed as they age and interact with health and care systems. There is an opportunity for the NHS and local authorities to support or mandate training for employees (including on the impact of stigma), linking to wider partnerships such as the Fast Track Cities initiative.
NES is working to update materials and training targeted at healthcare practitioners in non-HIV specialist roles and a specialist educator post has been funded by Scottish Government to support the provision of training across Scotland. This work may need expanding, and other partners (such as Fast Track Cities) may also have a role in developing training.
HiTEOG 2.4: To support public facing information to increase understanding and knowledge of HIV and to reduce stigma given the impact of effective treatment and prevention.
Action 2: A comprehensive anti-stigma campaign to the general public and groups with higher prevalence of HIV, to be delivered via social, web, out-of-home and TV media.
Delivery by: Terrence Higgins Trust (THT) Scotland partnered with NHS, PHS, third sector organisations and academia and funded by Scottish Government.
Timeline: Short term Completed: January 2024 - with evaluation to follow.
Details: In February 2023 Scottish Government commissioned a multi-agency partnership led by THT Scotland, to deliver a campaign aimed at reducing stigma in the general public. This multi-platform campaign[vii] was launched in October 2023 aiming to influence the knowledge, attitudes and behaviours of the population as a means of reducing the HIV-related stigma experienced by people living with both diagnosed and undiagnosed HIV, and people most at risk of acquiring HIV. A secondary goal was to reduce barriers to HIV prevention interventions. The campaign will be evaluated and should form the basis for further anti-stigma work. Other stigma work such as that carried out through Fast Track Cities should also continue.
Action 3: To review the potential costs and benefits of a HIV Testing Week.
Delivery by: Scottish Government
Timeline: Longer term. Commence: 2025/26
Details: The scoping group gave serious consideration to a Scottish HIV Testing Week but overall, it was felt that the benefits in terms of addressing stigma and promoting testing were better achieved through existing and planned awareness raising campaigns and the promotion of testing year-round. This should be reviewed once priority actions to expand capacity and improve access to testing have been progressed. The review should consider evidence of the effectiveness of similar campaigns elsewhere, not only on testing uptake but the number who have never tested before and the number of new diagnoses.
HiTEOG 2.5: To align teaching content in Scottish educational settings and in the Curriculum for Excellence to reflect updated HIV transmission risk and the reality of living with HIV in current times.
Action 4: Work with education policy to develop and update teaching resources as appropriate.
Delivery by: Scottish Government
Timeline: Medium term. Commence: 2024/25
Details: As we work towards HIV transmission elimination it is important that school-based education reflects the current realities of HIV and that resources are accurate, non-stigmatising and reflective of risk. We will work to ensure that updating this information is included as part of work to update Relationships, Sexual Health and Parenthood Education and consider if further resources are needed beyond this.
HiTEOG 3.1: To create an implementation group to disseminate updated HIV pre-exposure prophylaxis (PrEP) prescribing guidance, provide training to prescribers, roll-out awareness resources and deliver PrEP preparedness.
Action 5: Review BASHH/BHIVA guidelines on PrEP suitability for appropriateness of use in Scotland, endorsing and working with PHS to publish an addendum if appropriate and required. NES will review, update and disseminate training materials.
Delivery by: HIV-TEDI, PHS and NES.
Timeline: Short term Commence: October 2023 Complete: June 2024
Details: Existing eligibility criteria for PrEP need to be updated to ensure that the benefits of PrEP reach wider groups in addition to gay, bisexual and other men-who-have-sex-with-men (GBMSM). Revised Scottish PrEP Guidance was developed in parallel with updating of the current British Association for Sexual Health and HIV (BASHH) and British HIV Association (BHIVA) PrEP Guidelines[viii]; which should be published in 2024. New and updated training materials to be delivered through online education portal TURAS should also be rolled out. This will constitute an initial step in widening PrEP access, but more work will be required to ensure PrEP equity for all populations across Scotland.
HiTEOG 3.2: To estimate the characteristics and number of additional individuals likely to initiate PrEP in primary care settings (such as community pharmacies and general practice).
Action 6: Review existing evidence and evaluate pilot projects to establish the number of individuals likely to initiate PrEP.
Delivery by: HIV-TEDI and Scottish Government.
Timeline: Beyond 2025/26
Detail: It was recognised by the PrEP SLWG that estimating with any degree of robustness, the proportion of people underserved by current PrEP provision who would access PrEP through non-sexual health settings is unfeasible. Given the limitations and challenges of estimating the number of individuals likely to start PrEP in primary care settings, it is likely that data collection from and robust evaluation of pilot projects will be the most effective way of determining the preferred approach. Pilot services should include an assessment of potential uptake if this is appropriate for the service and evaluation design. This recommendation will be reviewed in the next iteration of the Delivery Plan to be developed in 2025/26.
HiTEOG 3.3: To explore the acceptability and feasibility of alternative community-based PrEP access and delivery models for people whose needs are not being met by existing arrangements in specialist sexual health settings.
Action 7: PrEP Workshop to be carried out to identify further PrEP actions.
Delivery by: HiTEOG short-life PrEP delivery subgroup.
Timeline: Short term Completed: April 2023
Details: A workshop on ‘Developing PrEP care models for diverse needs in Scotland’ was held in March 2023. A comprehensive evidence summary and report on the workshop was produced in April 2023[ix]. International evidence shows that initiating and maintaining PrEP supply to all those who need it is challenging, but outreach models have been successfully delivered and evaluated in Scotland[x] and recognised as good practice by the World Health Organization (WHO)[xi] [xii]. The scoping group identified that an important additional consideration is the retention in and re-entry into care of all PrEP users. Work to ensure that PrEP users continue to be linked to care, and to re-engage those who have stopped attending services but still need PrEP will be an important additional priority in the Delivery Plan. The workshop report has identified a number of actions to be taken forward under this recommendation which are captured in actions 8–12.
Action 8: ePrEP pilot to be funded and taken forward in Scotland.
Delivery by: Glasgow Caledonian University, Scottish Government.
Timeline: Short term Commence: December 2022 Complete: December 2025
Details: In December 2022, Scottish Government announced funding of £400,000 for a 36 month programme of work led by Glasgow Caledonian University (GCU) to develop and pilot an ePrEP clinic[xiii]. This aims to provide an efficient care pathway for people with straightforward PrEP needs to self-manage a proportion of their PrEP care. This work has begun and important groundwork is underway to ensure the pilot is safe and acceptable to users. The ePrEP pilot will continue to be taken forward during 2024 and 2025.
Action 9: The development of public and professional facing information on PrEP, to reflect the revised prescribing guidance.
Delivery by: Waverley Care and partners.
Timeline: Short term Completed: June 2023 – update as required.
Details: Video resources were co-developed with clinicians and community members by a team supported by GCU and Waverley Care[xiv] in 2023. These may need updating to reflect other changes in guidance.
Action 10: Further exploration of the potential for Primary Care and Community Pharmacy to contribute to PrEP delivery, which may take the form of a workshop or Short-Life Working Group. Also to review PrEP Licensing status and potential to widen prescribing options to pharmacies and general practice.
Delivery by: Scottish Government.
Timeline: Short term Commence: October 2023 Complete: Beyond 2025/26.
Detail: The Scottish Government has allocated funding to NHS Grampian and Aberdeenshire Health and Social Care Partnership to explore the feasibility and acceptability of HIV PrEP provision in primary care in the Northeast of Scotland. This project will be taken forward through 2023-25 with learning considered beyond the pilot. Work to explore the feasibility of provision within community pharmacy will also need to be considered during 2024/25.
Further work is also required to consider the implications of the current licensing status of PrEP which restricts prescribing to specialist sexual health services and to further explore the potential for prescribing in Community Pharmacies and General Practice and other settings to support equity of PrEP access. Work on resolving these issues will be scoped during 2025/26, however this may take longer to fully resolve.
Action 11: Outreach models for populations who have barriers to PrEP access and/or a higher prevalence of HIV infection will be considered by HIV-TEDI with pilots taken forward when feasible.
Delivery by: HIV-TEDI to advise.
Timeline: Medium term Commence: 2024/25
Details: HIV-TEDI to advise on potential work to be taken forward to further this action drawing on internationally recognised examples of good practice such as the PrEP service tailored to the needs of people who inject drugs in Glasgow[xv].
Action 12: Develop a PrEP intervention for transgender people.
Delivery by: TBC
Timeline: Beyond 2025/26
Details: This intervention, recommended by the HiTEOG short-life PrEP delivery subgroup, will need to carefully consider wider healthcare needs of trans people, particularly those awaiting gender-affirming healthcare. This will be developed for the next iteration of the Delivery Plan to be developed in 2025/26.
Contact
Email: SHBBV@gov.scot
There is a problem
Thanks for your feedback