Stabilisation, detoxification and other crisis support in Scotland: Service mapping and capacity survey 2022/23
This report presents the findings of from a survey of stabilisation, detoxification and other crisis support providers in Scotland.
3. Results
The main survey received 80 responses. Ten invalid responses were removed and duplicate returns from the same organisation were consolidated into a single response, resulting in a total of 65 responses for analysis.
Responses to the prison survey were received from 12 of the 15 Scottish prisons. As these results cannot be directly compared to those of community-based or other residential services, the findings are reported in the final section of this report.
3.1 Stabilisation
The results of this survey indicate a variation in how stabilisation is understood and interpreted by respondents. Respondents were asked to provide information on the treatment and support they offered.
For the purposes of this survey, providers were classed as offering a form of stabilisation if they reported offering opioid substitution therapy (OST) and/or benzodiazepines and/or OST optimisation. A total of 38 providers were identified as offering these services. It should be noted that 10% (n = 4) of the providers classed as providing stabilisation using this definition did not self-describe as doing so.
3.1.1 Types of providers
Stabilisation is offered across a range of organisation types. Due to the question format in the survey, it is not possible to entirely categorise these as statutory, private and third sector organisations. However, about two thirds of services responding to the survey (71%) were statutory organisations (either NHS hospitals or other statutory organisations), 16% were residential rehabilitation providers[2] and 8% were third sector organisations. The remaining 6% were a general practice and a private hospital.
3.1.2 Geographic distribution and model of delivery
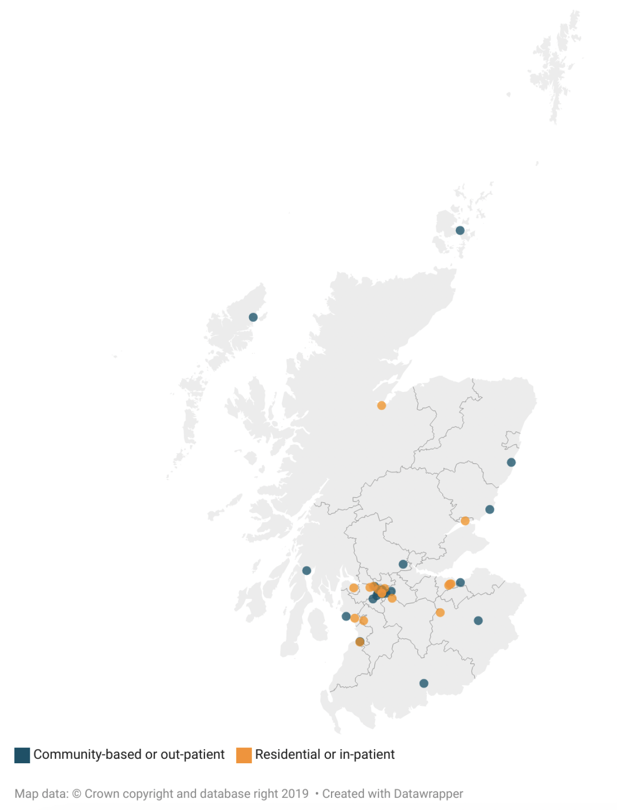
There is a fairly even division in the model of delivery for these services. Around half of providers (53%, n = 20) operate a community-based or outpatient model of delivery.The other half of providers operate in a residential or in-patient setting,with one provider describing a hybrid model of community-based delivery with access to specialist NHS acute hospital beds.
Glasgow City has the highest concentration of both residential and community-based services, with around a third (34%, n = 13) located in this local authority area (Figure 1). The other 25 services were spread across 20 local authority areas. Three are in the City of Edinburgh; two each in South Ayrshire, East Ayrshire and the Scottish Borders; and one in each of the following local authorities: Aberdeenshire, Angus, Argyll and Bute, the Western Isles, Dumfries and Galloway, Dundee City, East Lothian, East Renfrewshire, Highland, Inverclyde, North Ayrshire, Orkney, Renfrewshire, South Lanarkshire, Stirling and West Dunbartonshire.
Figure 1: Location of residential and community-based stabilisation providers in Scotland
3.1.3 Capacity estimates
The survey included questions aimed at compiling an estimate of the stabilisation capacity across Scotland. However, analysis indicated that a lack of common understanding or definition of stabilisation and differences observed across the models of delivery make the interpretation of this data challenging. For example, capacity was often reported as having no upper limit and no clear distinction was made between capacity for different types of treatment. This indicates that this question was interpreted as the total number of people a service can accommodate and that resources within an organisation can be flexed to meet demand/ needs of people presenting for treatment. This is indicative of a person-centred approach being adopted across services, such that an assessment of a person's needs determines the type of treatment or support provided. While further research will be required to better understand this, data on the current number of people attending services can provide an indication of current capacity, assuming demand is sufficiently high. It should be noted that this data can only provide a snapshot of the current levels of attendance to these services at the time of the survey.
Of the 29 providers that provided an estimate, there was a total of 272 people attending residential or in-patient services and 1,603 people attending community or out-patient services[3]. The estimates provided varied considerably between 2 and 61 people for residential or in-patient services; and between 10 and 500 for community-based or out-patient services. Nine respondents (primarily from services operating in a community-based or out-patient setting) indicated that they were not able to provide this due to the variation in the number of people using their services month on month, or issues around accessing this data.
3.1.4 Treatment and support
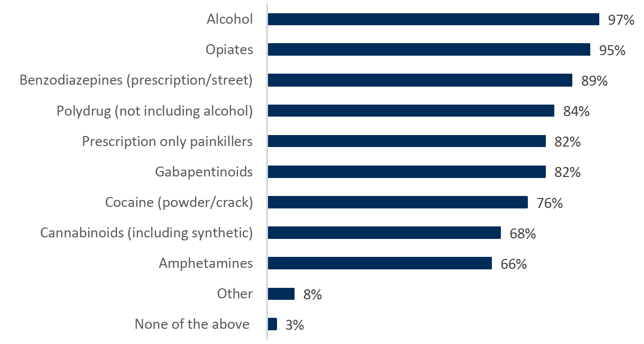
Providers offer treatment for a range of substance use profiles (Figure 2). Most providers are able to offer treatment or support for the use of alcohol (97%), opiates (95%) and benzodiazepines (89%). Other substances mentioned included performance and image enhancing drugs (n = 1) and ketamine (n = 1).
Figure 2: Share of providers reporting offering treatment or support by type of substance
The mapping survey identified a total of 38 services providing some form of stabilisation. The majority of services (74%, n = 28) reported offering OST prescription, benzodiazepine prescription and OST optimisation. The remaining ten providers offer a single or combination of these three services. When offering just one of these services, this is always in combination with some form of detoxification and/or behavioural or psychological intervention:
- Prescription of OST – 2 providers
- Optimisation of OST – 1 provider
- OST and benzodiazepine prescribing – 4 providers
- OST prescription and optimisation – 2 providers
- Prescription of benzodiazepines – 1 provider
Almost all (95%, n = 36) also offer some form of detoxification. Detoxification from both alcohol and drugs is most common (79%, n = 30), but five are limited to alcohol and one to drugs.
A range of other treatment and support is available across these 38 providers:
- All but one (n = 37) reported providing naloxone.
- An active connection to community recovery resources (e.g. mutual aid) is offered by 95% (n = 36) providers.
- Blood-borne virus testing and behavioural or psychological interventions are offered by 92% (n = 35) of providers. Behavioural and psychological interventions included techniques such as motivational interviewing, brief interventions, cognitive behavioural therapy (CBT), Eye movement desensitisation and reprocessing (EMDR), therapeutic community, trauma-informed. An intervention referred to as "safety and stabilisation" was also mentioned by some providers. These interventions were described as ranging from low intensity group interventions (sometimes described as Tier 1) to specialist one-to-one interventions (sometimes described as Tiers 3 and 4) with support from specialised mental health staff (e.g. psychologist, psychiatrist, mental health nurses, key workers, etc.).
- Provision of alcohol relapse prevention medication is offered by 87% (n = 33) of providers.
- Wound care is offered by 76% (n = 29) of providers.
- Sexual health care is offered by 58% (n = 22) of providers.
- Dental care is offered by 8% (n = 3) of providers.
- One provider also reported offering injection equipment provision (IEP), and another also reported offering physical fitness related therapies (e.g. yoga).
3.1.5 Duration of treatment
The treatment and support services offered by the stabilisation providers ranged considerably in length from a few days to having no real upper limit, largely depending on the model of delivery. Providers operating in a residential or in-patient setting reported treatment lengths of between 5 days and 10 months, with residential rehabilitation providers generally reporting the longest period of treatment (ranging between 7 days to 10 months). NHS hospital in-patient services tended to have shorter periods of treatment (ranging between 5 days and 3 weeks), although a private hospital reported a length of 6 weeks.
Community-based providers all reported longer treatment times of between 6 weeks and several years. Several respondents indicated that this was largely dependent on the treatment offered, with open-ended support being common for patients on long-term OST.
3.1.6 Waiting lists and waiting times
Most providers (68%, n= 26) do not operate a waiting list for their services. The 12 providers that do have waiting lists described waits of between two weeks and up to 12 weeks, although a few noted that this varies depending either on capacity or clinical need.
3.1.7 Exclusion and screening criteria
About two thirds (63%) of the respondents stated that there are no criteria for exclusion from their service. Where exclusion criteria were noted, these included the profile of substance use (11%), the existence of a criminal record (8%) or of a specific mental health concern (5%), and an individual not being considered at a point of crisis with regard to their substance use (3%). A few respondents specified that people are assessed on a case-by-case basis and that these criteria might not necessarily result in automatic exclusion from the service. A few respondents also mentioned that people presenting with a mental or physical health condition requiring medical attention or best suited to another service would potentially delay, although not necessarily exclude, someone from admission to their service.
3.1.8 Referral pathways
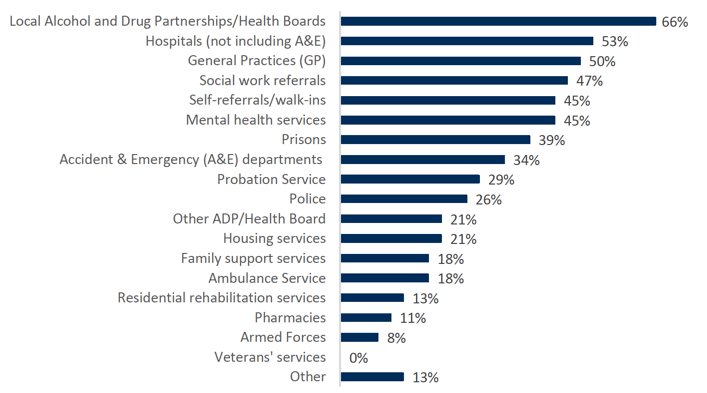
People arrive at the services via a range of different referral pathways (Figure 3). Around half of respondents also said people 'often' or 'always' come from the local ADP or Health Board area (53%), hospitals (50%), general practices (47%) or through social work referrals (45%). It is also quite common for people to self-refer to the services, with 45% of providers saying this is 'always' or 'often' the case. Referrals from other ADP or Health Boards, the Ambulance Service, and family support or housing services were less likely.
Figure 3: Share of providers responding that their service users 'always' or 'often' arrive to their service by type of pathway
3.1.9 Staffing
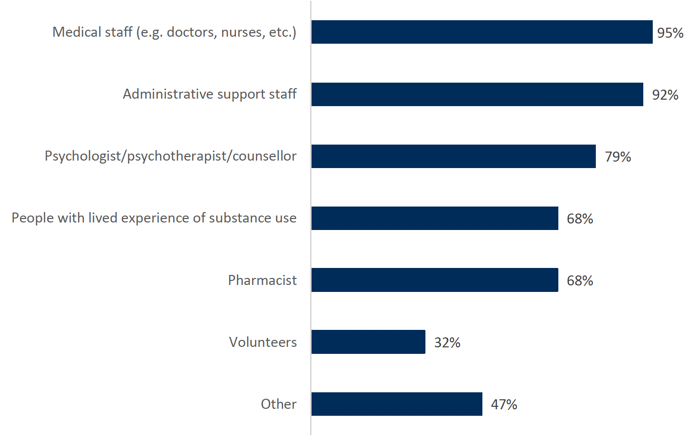
The services employ staff across a range of professions (Figure 4). While about a third (32%) of services have volunteers, the majority operate with salaried staff. The most common are medical staff (95%) and administrative support staff (92%) as well as 79% being mental health professionals (psychologists, psychotherapists or counsellors). People with lived experience were reported to be employed by 68% of providers. Other professions employed include occupational therapists, social workers, mental health nursing staff, and support workers.
Figure 4: Share of providers reporting employing different professions (in a paid or volunteer capacity)
3.1.10 Regulatory frameworks
All of the 38 services operate within one or more regulatory frameworks. Most (79%) are regulated by the National Health Service (NHS), about half (47%) are regulated by Healthcare Improvement Scotland (HIS), and about a third (34%) by the Care Commission.
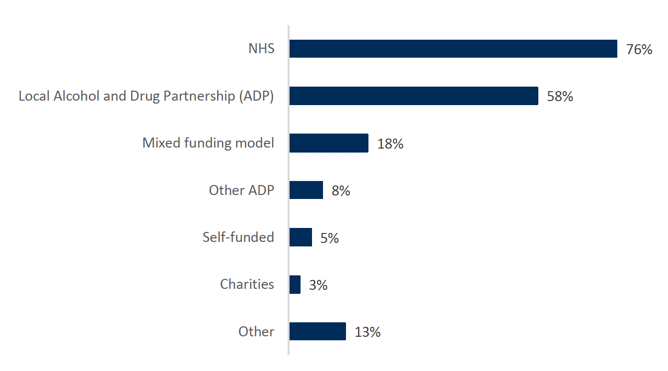
3.1.11 Funding sources
Funding for people using these services comes from a range of sources (Figure 5). The most common source of funding is through the NHS or local ADPs, with 76% and 58% of respondents reporting that this is 'always' or 'often' the case. It should be noted that these estimates may have been slightly inflated by the 18% of providers that reported having mixed models of funding.
Most providers reported that self-funding is uncommon, with 84% saying that this is never the case. Other sources of funding mentioned included, local authorities and the Scottish Government[4].
Figure 5: Share of providers responding that their service 'always' or 'often' receive funding by source of funding
3.1.12 Service user outcomes
Providers were asked how they measured outcomes for people using their services. Outcome Star or DAISy were most commonly said to be used by those who responded to this question, although a few also reported using other questionnaires or surveys. Some providers reported that measuring outcomes is not yet commonplace but is in development.
People are most commonly reported to return home following discharge from a residential service, with 94% of these providers saying this is 'always' or 'often' the case. Hospitals also reported that common routes upon discharge include a move to other wards or a transfer to community services. A move to some form of supported accommodation was also mentioned as being common by residential rehabilitation providers and third sector organisations.
A placement in residential rehabilitation is not a common next step, with almost two thirds of residential providers (65%) and three quarters (75%) of community-based providers responding that service users 'rarely' or 'never' move on to this following discharge from their service.
3.2 Detoxification services
The mapping survey identified a total of 41 services providing detoxification in Scotland, based on having selected 'detoxification from alcohol' AND/OR 'detoxification from drugs' from a list of treatments offered. The majority (n = 36) also offer some form of stabilisation and have been discussed above.
The five remaining detoxification providers identified come from a range of organisations. Three are residential rehabilitation providers, one is a community alcohol detoxification team, and one is a homelessness service (therefore split between operating on a residential or community-based context).
Three offer both alcohol and drug detoxification, one only drugs and one only alcohol. All also offer behavioural or psychological interventions and an active connection to community recovery resources.
3.3 Other crisis support services
A total of 24 providers were identified as offering another form of crisis support, which did not include stabilisation and/or detoxification. These were primarily third sector or homelessness services principally operating in community-based settings (75%). The majority of providers (71%) reported that all or more than half of their services are specifically dedicated for people at a point of crisis with regard to their substance use.
A range of other treatment and support is available across these providers. Ten of these services describe themselves as offering stabilisation, all had active connections to community recovery resources and 60% offered behavioural or psychological interventions.
- Most (88%, n = 21) reported providing naloxone.
- An active connection to community recovery resources (e.g. mutual aid) is offered by 79% (n = 19) providers.
- Behavioural of psychological interventions are offered by 58% (n = 14) of providers. The interventions described were generally low intensity psycho-social ones with no mention of specialist mental health staff. They included peer support groups and techniques such as motivational interviewing and cognitive behavioural therapy (CBT).
- Blood-borne virus testing is offered by half (n = 12) of providers.
- Wound care is offered by about a third (29%, n = 7) of providers.
- Sexual health care is offered by 17% (n = 4) of providers.
- Other services also included harm reduction advice or unspecified harm reduction (4 providers); IEP provision (1 provider); wound care, assessment of injecting risk, naloxone and dry blood testing (1 provider); educational activities for young people (1 provider).
3.4 Prisons
3.4.1 Treatment and support programmes
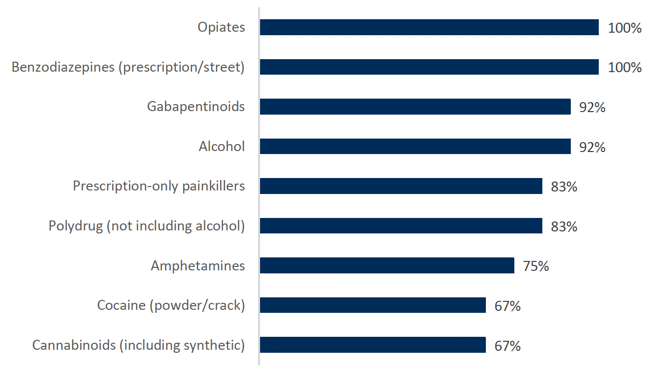
Prisons provide treatment across the range of substance use profiles (Figure 6).All offer treatment for opiates and benzodiazepines and over three quarters (between 75-92% depending on the substance) offer treatment across the rest of the substance use types. Cocaine and cannabinoids are the least common substances for which treatment is offered, however the majority (67%) of prisons still report doing so for both of these.
Figure 6: Share of prisons reporting offering treatment or support by type of substance
All prisons offer some form of stabilisation. Three quarters (75%, n = 9) reported offering OST prescription, benzodiazepine prescription and OST optimisation. The remaining three prisons offer a single or combination of these three services.
- Prescription of OST – 1 prison
- OST prescription and optimisation – 2 prisons
All but one prison (92%, n = 11) also offer some form of detoxification. Detoxification from both alcohol and drugs was most common (83%, n = 10), with one prison only offering detoxification for drugs. A few respondents noted in open-text answers that detoxification is only provided to new arrivals to the prison.
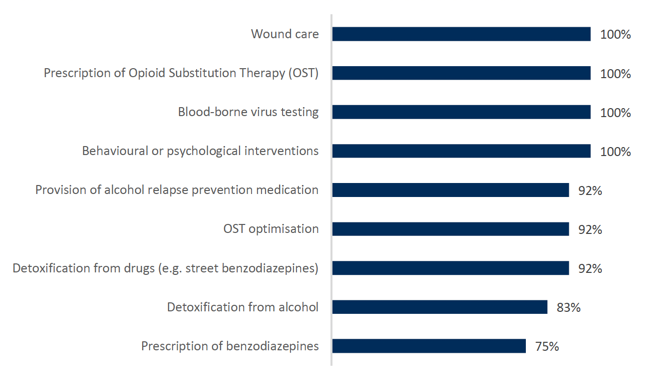
All prisons also reported providing wound care, blood-borne virus testing and behavioural or psychological interventions (Figure 7).Behavioural and psychological interventions included techniques such as motivational interviewing, cognitive behavioural therapy (CBT), relapse prevention and trauma-informed care. An intervention referred to as 'safety stabilisation' was also mentioned by a couple of respondents. These interventions were described as ranging from low intensity interventions with members of the addiction team or nurses to specialist one-to-one interventions (sometimes described as Tier 3), potentially with support from specialised mental health staff (e.g. clinical psychology team).
All but one prison also provides alcohol relapse prevention medication. Follow-up conversations by emails, telephone or Microsoft Teams were held with respondents from four different prisons to clarify how naloxone is used in Scottish prisons. While in prison, naloxone is not distributed to prisoners but is available to members of the prison staff (in its intranasal form) and healthcare staff (in its injectable form) for use in the event of an overdose. Naloxone is offered to people upon release from prison and respondents described different arrangements for delivering training prior to release and maximising uptake of take-home naloxone upon release.[5]
Figure 7: Share of prisons by type of treatment or support offered
3.4.2 Capacity
As for the general population, while a couple of respondents attempted to provide an estimate for the maximum capacity at their prison, almost all of the respondents to this survey reported that a patient-centred approach is taken and that there is no maximum capacity. Instead, treatment and support are delivered based on an assessment of need when new arrivals to the prison come in.
Contact
There is a problem
Thanks for your feedback